The ARS medical company has procured Olympus EVIS EXERA III the most up to date, latest generation video endoscopy equipment in the world. Thus becoming the only medical centre in the Baltic States with this technology.
The EVIS EXERA III is made by Olympus technology research and development specialists in collaboration with the world’s leading gastroenterology and endoscopy doctors. The devices optical and digital specifications have revolutionised endoscopic examinations bringing in new standards that will positively influence examinations and medical treatment opportunities in the future.
The new Olympus EVIS EXERA III presents unique and novel diagnostic opportunities, which are particularly fundamental for early gastrointestinal disease and new growth detection and therapy.
Most important innovations:
- High resolution digital imaging that enables the detection of even the most minuscule changes to the structure of the mucous membrane;
- Makes it possible to thoroughly inspect tissue in revolutionary proximity – 2 mm distance from the wall of the mucous membrane;
- If necessary, images can be enlarged during an examination up to a cellular level;
- It is possible to look at mucous with a proprietary Olympus technology called “Narrow Band Imaging” (NBI), that enables capillary network evaluation and the identification of pathological tissue from normal tissue at the very beginning of illness;
- A substantially improved user interface makes the examination more pleasant for both the doctor and the patient;
- A wide range of image documentation and comparison possibilities.
Narrow band imaging (NBI) mode enables the evaluation of the intestinal mucous membrane. This mode enables differentiating between the pathological mucous membrane from the normal one by analysing capillary networks at the very early stages of illness.
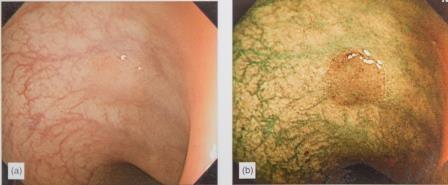
Images show the same intestinal mucous membrane:
a) A mucous membrane without any visible pathologies;
b) The same mucous membrane with pathological changes, using Olympus EVIS EXERA III NBI mode.
What kind of examinations is it possible to perform with the Olympus EVIS EXERA III endoscope?
Upper GI endoscopy or in other words Gastroscopy.
It is possible to perform Upper GI endoscopy or in other words Gastroscopy (oesophagus, stomach and duodenum examination). This is the most precise method for early diagnosis and treatment of the gastrointestinal tract. During the procedure an optical device – flexible tube, which has a light source and a camera attached to its end – is passed through the patient’s mouth and into the digestive system. It allows a detailed image inspection on the monitor of oesophagus, stomach and duodenum mucous membranes. If a detailed examination of a particular area is necessary, enlarging the image to the cellular level is possible. The Endoscope canal can also be used to perform diagnostic and medical manipulations, for example to remove polyps, treat bleeding ulcers or perform a biopsy (take a tissue sample of the mucous membrane to evaluate cancer risk).
When is it necessary to perform gastroscopy?
Gastroscopy examinations are done if patient complains about difficulty swallowing, pain and a burning sensation in the stomach, pain in the upper part of the stomach, vomiting blood. It can also be used if there are suspicions of ulcer formation, during follow-up ulcer treatment and in cases when tumour growth risk needs to be assessed.

At the end of the endoscope there are optical lenses and a source of light with different light filter modes that allow the investigation of the GI tract to a cellular level.
Preparation for the gastroscopy examination:
- The patient must arrive with an empty stomach for the examination!
- A light dinner is advisable, no later than 8pm the night before. Still water and tea are allowed after dinner.
- No drinking, eating or smoking is permitted on the day of the examination.
- Anaesthetic will be administered intravenously before the examination to facilitate the procedure and relieve unpleasant sensations. It also ensures a higher quality procedure.
Lower GI endoscopy – Colonoscopy (examination of the large intestine).
This procedure is performed through the anus. An optical device – a flexible tube that has a light source and a camera attached to its end – is used for colonoscopy, which allows for a detailed image inspection of the large intestine mucous membrane on the monitor. If detailed examination of a particular area is necessary, enlarging the image to a cellular level is possible.
The new colonoscope is equipped with an improved endoscope entry component to make the procedure gentler. This greatly improves the examination experience for both doctor and patient. A high resolution and improved conduction technology allow doctors to use this new generation endoscope to efficiently evaluate the mucous membrane of the large intestine and rectum. The improvements make it virtually impossible to miss any pathological changes. It is also possible to perform various diagnostic and medical manipulations during colonoscopy, such as taking samples of the mucous membrane for analysis, performing polypectomy (removal of polyps) and stop internal bleeding.
When is it necessary to perform a colonoscopy?
A Colonoscopy is performed on patients who have: disrupted bowel movements – chronic constipation or frequent diarrhoeas, passing stools containing blood, constant abdominal bloating, pain in the lower abdomen, cases of colorectal cancer in the family medical history and for elderly people. Several conditions can be diagnosed through colonoscopy including haemorrhoids, polyps and the evaluation of risk factors in colorectal cancer progression. It is common practice for gastroenterologists, gynaecologists, proctologists and other specialists to advise colonoscopy examinations for their patients. It is done in order to diagnose diseases of the colon as well as the progression of malignant tumours.
RECOMMENDATION: it is proposed that everyone over the age of 50 should undergo a colonoscopy – the examination of the large intestine and rectum – in order to disclose any pathological changes at their early stages.
Preparation for the colonoscopy procedure
- The cleaner the intestine, the better quality the diagnosis will be. There is little point in performing the colonoscopy if intestines are not clean.
- Only a light breakfast is allowed the day before the colonoscopy examination. After breakfast comes a period of fasting and consumption of special intestine cleaning fluid. However, still water and tea is allowed in unlimited amounts.
- Patients need to purchase an intestine cleaning agent “Fortrans” (contains 4 packets of the medicine) or a medicine named “Cololyt” that is sold in bottles. Carefully read the instruction before using!
- Before the colonoscopy examination, it is necessary to empty your bowels in the bathroom for the last time.
- Only those medicines that are prescribed for a regular use can be taken on the day of colonoscopy, for example – medicines to treat high blood pressure.
Pain relief
To lower and extinguish any discomfort or feeling of fear, the upper GI endoscopy can be performed under light anaesthesia. However, patients can opt for a deeper form of anaesthesia. For colonoscopy the anaesthetic is administered intravenously (if patients wish), rendering the procedure painless. The narcosis is very light and short-term to reduce any discomfort. The procedure is supervised by a certified anaesthesiologist.
Warning: it is recommended not to drive or to handle machineries that require high level of concentration and precision for 12 hours after the administration of anaesthetics, as medicines can cause sleepiness as well as reduce attention and concentration.
For your knowledge:
To be able to undergo these procedures a referral note from a specialist doctor is necessary. This service is paid for by insurance agencies.
Gastroscopy and colonoscopy examinations are performed by:
Gastroenterologist, endoscopist Dr Anita Lapiņa;
Gastroenterologist, endoscopist Dr Andra Altberga;
Gastroenterologist, endoscopist Dr Dabri Abdul Massih.
To sign up for an examination, please call:
+371 67201006;
+371 67201007;
+371 67201008.




